6 Classic Bands That Influenced Today’s Music
In the 60s and 70s, many bands became famous for producing music that resonated with the people. A few of them were so unique and inventive in their musical style that they became an inspiration for f...
Aging is a natural process that brings many changes to your body and mind. Some of these changes are expected, such as gray hair and wrinkles, but some are unexpected, such as joint pain, stiffness, and swelling. These symptoms are often from a medical condition called arthritis, which affects about 528 million people.1
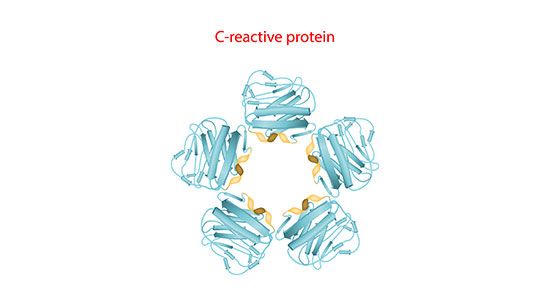
If you’ve recently been diagnosed with arthritis, you may have heard about a blood test to measure C-reactive protein (CRP) and wonder what this test has to do with your condition.
In this article, we’ll explain what CRP is and discuss its link to arthritis. We’ll also share recent studies on aging, CRP, and arthritis, which have provided insights into the role of inflammation in aging.
CRP belongs to a group of proteins known as acute-phase reactants. As a response to inflammation,2 your liver produces CRP and releases it into the bloodstream.
The role of CRP is to activate certain parts of your immune system, specifically white blood cells called macrophages, to help clear foreign attackers and dying or dead cells from the body.
Another function of CRP is to bind to the surface of some bacteria, making it easier for your immune system to recognize and destroy.
CRP levels rise and fall with changing levels of inflammation in the body,3 making CRP an ideal marker for inflammatory conditions. Inflammatory markers, including CRP, are blood tests that detect inflammation in the body.
Evidence-based insights into the role of C-reactive protein and arthritis:
Arthritis, particularly rheumatoid arthritis, can cause high CRP levels due to systemic inflammation.
Additionally, arthritis can indirectly influence CRP levels by affecting your overall health and well-being. It can limit your physical activity levels, impair your sleep, and disrupt emotional wellness. All of these factors can contribute to increased inflammation in your body and an elevated CRP level.3
Labs interpret CRP levels in either mg/dL or mg/L. Below is a chart showing standard lab values5 and what they indicate.
| Level | Elevation level | Possible Condition |
| Less than 0.3 mg/dL | Normal | Healthy |
| 0.3 to 1.0 mg/dL | Normal or minor | Pregnancy, common cold, periodontitis, gingivitis, unhealthy lifestyle habits, sedentary lifestyle, or genetic polymorphisms |
| 1.0 to 10.0 mg/dL | Moderate | Rheumatoid arthritis, lupus, other autoimmune diseases, cancer, myocardial infarction, bronchitis, or pancreatitis |
| More than 10.0 mg/dL | Marked | Acute bacterial infection, viral infection, systemic vasculitis, or major trauma |
| More than 50.0 mg/dL | Severe | Acute bacterial infection |
What level of C-reactive protein indicates rheumatoid arthritis? A level between 1.0 to 10.0 mg/dL5 indicates systemic inflammation, such as rheumatoid arthritis.
Understanding the role of inflammation as you get older is essential for treating and preventing many age-related diseases.
Inflammation is a natural defense mechanism that helps your body fight infections and heal injuries. However, as you get older, your immune system becomes more prone to chronic, low-grade inflammation that damages your cells and tissue. This type of age-related inflammation is known as inflammaging.7 It is associated with almost all age-related diseases, including arthritis, type 2 diabetes, cardiovascular disease, and cancer.
Recent studies on aging, CRP, and arthritis have provided some insights into the role of inflammation, including:
C-reactive protein levels between 1.0 and 10.0 ml/dL are moderately elevated and signal systemic inflammation in the body, such as rheumatoid arthritis.
CRP levels above 10 ml/dL are markedly elevated and may indicate severe infection or trauma.
CRP levels above 50 ml/dL5 are considered severely elevated and are often associated with a bacterial infection that requires immediate medical attention.
If you have rheumatoid arthritis, your doctor may order a simple blood test to check your CRP level and other inflammatory markers such as erythrocyte sedimentation rate (ESR) and rheumatoid factor.
They may also order a specific CRP test, hs-CRP, to assess your risk of cardiovascular disease.
Depending on the results of these tests, your doctor may recommend treatment options to reduce inflammation and lower your CRP levels.
Regular monitoring of your CRP levels can help doctors evaluate the effectiveness of your treatment plan. Changes in CRP levels may warrant a tweak in your treatment plan.
Making simple lifestyle changes can help to manage your CRP levels and arthritis. Some tips for a healthy lifestyle include:
If you have arthritis, checking in with your doctor regularly for checkups and bloodwork can help monitor the effectiveness of your treatment plan. If your doctor finds irregularities in your exam or bloodwork, they can make necessary changes to your treatment plan to help manage your arthritis more effectively and improve your quality of life.
C-reactive protein is a marker of inflammation that can aid in diagnosing and monitoring arthritis, particularly rheumatoid arthritis. It can also help indicate your risk of cardiovascular disease, which increases with rheumatoid arthritis.
If you have arthritis, it’s important to regularly consult with your doctor for monitoring to determine the effectiveness of your arthritis treatment plan and make changes as needed.
Prioritizing a healthy lifestyle, including a balanced meal plan, regular exercise, stress management, and quality sleep as you age, can help to improve your quality of life and minimize the burden of arthritis.



Unlock expert insights and tips with our exclusive ebook. Enter your email to get your free copy.
Please check your email for a welcome message from Modern60. If it's not in your inbox, kindly check your spam or junk folder
There are no comments yet