6 Classic Bands That Influenced Today’s Music
In the 60s and 70s, many bands became famous for producing music that resonated with the people. A few of them were so unique and inventive in their musical style that they became an inspiration for f...
It can be difficult to know what to do when an elderly person doesn’t eat. But there is a way to help encourage them to eat and meet their nutritional needs. Eating issues are a common challenge among the elderly, affecting a significant portion of this population. Poor nutrition in older adults can have serious health implications, exacerbating chronic illnesses and contributing to a decline in overall physical condition.
By finding the cause of their loss of appetite, this can help to address that specific nutrition need. Here we will give you some reasons why they may refuse to eat as well as strategies to encourage intake.
If you’re still struggling, we warmly encourage you to reach out to a healthcare professional to address your concerns early. As an Registered Dietitian focused on senior nutrition for over 10 years, I’ve seen many older adults struggle with poor appetite and not eating enough. Let me give you my best advice for improving food intake in the elderly.

Many of the reasons that an elderly person won’t eat can be traced to a psychological, physiological, or social factor. Though it may seem as simple as encouraging them to eat more, the root cause of the appetite loss is important to address.
Some psychological reasons an elderly person may stop eating can include depression, anxiety, cognitive issues such as dementia or Alzheimer’s disease. A Doctor can help to diagnose and address these issues largely with counselling or medication.
A physiological reason an elderly person may not want to eat can be a complication of a new or recurrent disease condition they may have. If there is an acute issue such as pneumonia being treated, their appetite may decrease, but once the issue is resolved they will typically begin eating again. Similar to psychological causes, this should be investigated and treated by a Doctor to resolve the issue.
Social factors certainly play a role in an elderly individual not wanting to eat. This can be a variety of reasons such as not wanting to cook, limited access to healthy food, inability to go to a grocery store, or not having family around to help them. Issues that are socially related may need to be addressed through community resources and family support.
Age related factors also play a role in an elderly person not wanting to eat. Many of our senses tend to dull as we age such as taste and smell which can affect our desire to eat. Also a lack of physical activity can diminish our appetite, leading an elderly person to not wanting to eat.
All of these issues do need to be addressed not only to correct them, but also to come up with nutrition interventions that can address these root causes. Working with a healthcare team can really help to support an elderly person who doesn’t want to eat.
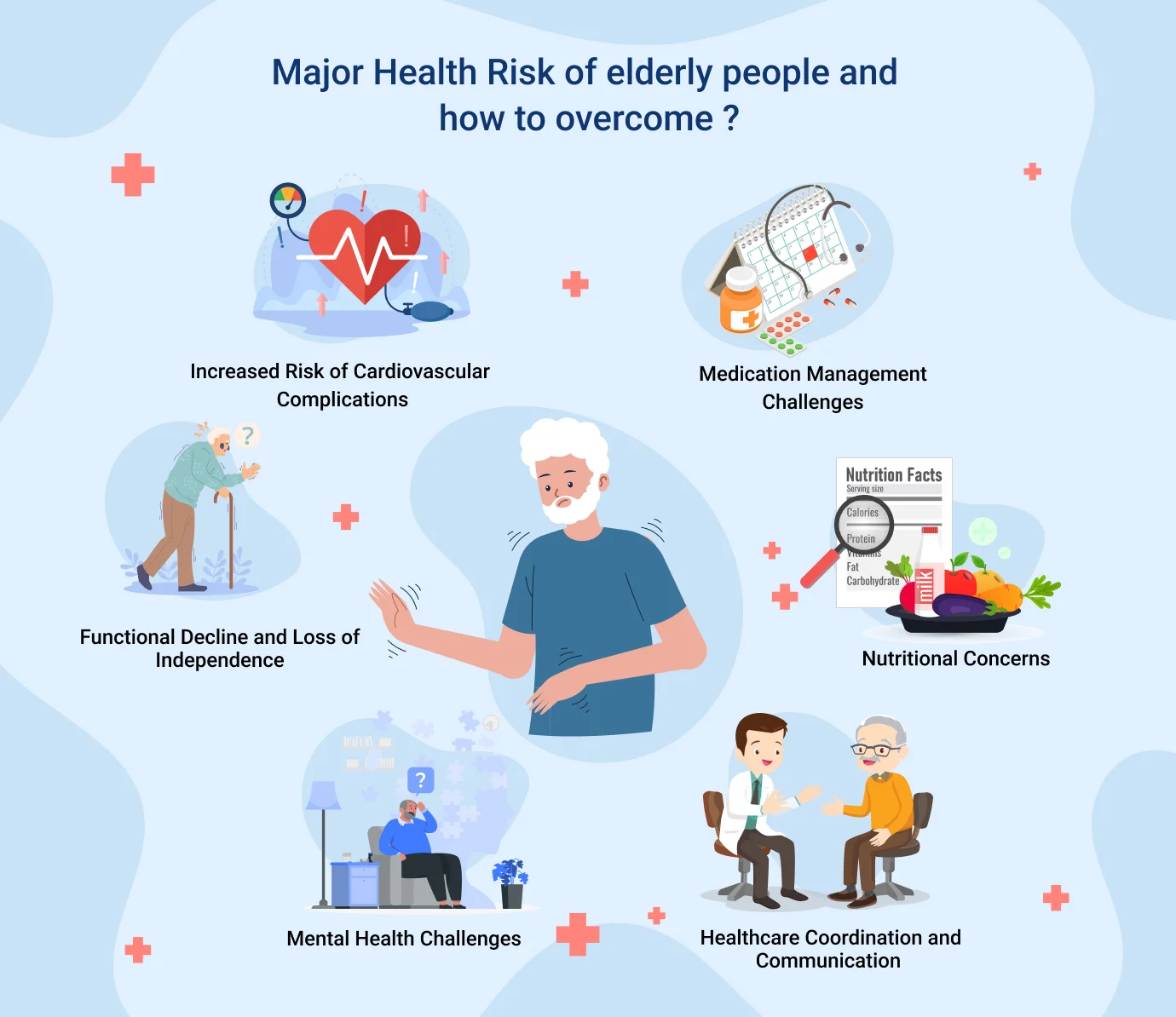
The reason that we need to address lowered food intake in an elderly person is that there are serious negative health consequences associated with it.
Elderly individuals are at higher risk of malnutrition, which is not eating enough to meet their needs. This can lead to poor wound healing, loss of independence, increased risk of falls and fractures, increased risk of hospitalisation and early mortality risk.
Ensuring that an elderly person is eating and drinking enough is the key to promoting a long life.
Muscle deterioration, or sarcopenia, is another significant risk. Without adequate protein and other essential nutrients, elderly individuals can experience a rapid decline in muscle mass and strength. This not only affects mobility and independence but also increases the risk of falls and fractures.
Overall decline in immune function is another critical concern. Nutritional deficiencies can impair the body’s ability to produce and activate immune cells, leading to a reduced ability to respond to pathogens. Long-term health consequences of poor nutrition include chronic fatigue, cognitive decline, and a higher likelihood of developing chronic diseases such as osteoporosis and cardiovascular issues. Addressing these nutritional issues promptly is essential to prevent these adverse outcomes and to ensure a better quality of life for elderly individuals.

Encouraging an elderly person to eat and drink nutritious things throughout the day to meet their needs is one of the keys to increasing their intake. Providing support for them can look like many different things.
Enhance Food Flavor: Providing them meals that are extra flavourful such as with herbs and spices, broths, and gravies can make food more appealing. This can help when their senses such as taste and smell are lacking.
Improve Visual Presentation: Creating a calm eating environment and reducing the amount of distractions can also help to increase their intake at meals. This may look like having a brightly lit dining room, calm quiet music in the background, no television on, and light conversations. This can help an elderly person to focus more on eating instead of being distracted.
Create a Pleasant Dining Environment: Making the dining experience a social experience has also been shown to increase the intake of elderly people at meals. Social meals include conversing with them whether this is talking about the food in front of them, or how their day went.
Offer Small, Nutrient-Dense Meals: Offering an elderly person smaller nutrient-dense meals can help them to increase their intake. Large meals can be overwhelming for an elderly person and actually discourage them from eating at all. Getting as much protein and calories as you can into smaller portions will help them meet their needs in a more efficient way as well.
Incorporate Favorite Foods: Include some of the elderly individual’s favorite foods in their diet to encourage eating. Familiar and preferred foods can boost appetite and make mealtime more enjoyable.
Use Soft and Easy-to-Chew Foods: For those with dental issues or difficulty swallowing, offer soft and easy-to-chew foods such as smoothies, mashed potatoes, pureed soups, and scrambled eggs. These foods are easier to consume and digest.

Trying to promote getting all their nutrition from food first is a great approach, but there may be times where they need help. Oral nutritional supplements can be a great way to help them meet their nutrient needs.
There are high-calorie high protein nutrition supplement drinks that are available at most stores that can help support the needs of elderly people. Elderly appetite loss can result in them not wanting to eat, sometimes a drink option can help to improve intake.
Common supplements include protein powders, meal replacement shakes, and fortified drinks like Ensure or Boost, which provide a balanced mix of vitamins, minerals, and macronutrients.
Before starting any supplement regimen, it is crucial to seek advice from healthcare professionals. Dietitians, doctors, and other healthcare providers can assess the individual’s nutritional needs, review any potential interactions with medications, and tailor recommendations to their specific health conditions. Always consult with a healthcare professional to choose the right supplement for your loved one if they need one. They can help to give caregiving tips for elderly nutrition to address the issue.

Coming up with elderly not eating solutions can require a team of healthcare professionals. A Doctor can help to determine what the root cause of the issue is for appetite loss. Seeking a Dietitian’s advice for elderly eating can help to give specific advice and develop a nutrition care plan that is specific to an elderly person once the root cause has been determined.
Working with a team of healthcare professionals is an excellent way to promote good food and fluid intake in elderly people.

Caring for an elderly individual who refuses to eat can be emotionally and physically demanding for caregivers. Managing stress and maintaining well-being is crucial to providing effective care. Here are some tips to help caregivers cope better:
Addressing the issue of elderly individuals refusing to eat requires a comprehensive approach that includes understanding the underlying causes, assessing nutritional risks, and implementing practical strategies to encourage eating. Nutritional supplements and professional guidance can play a crucial role in ensuring adequate nutrient intake.

Michelle Saari is a highly experienced Registered Dietitian based in Canada, specializing in nutrition for aging well. She holds a Master’s Degree in Human Nutritional Sciences from the University of Manitoba and has completed a Dietetic Internship at the Northern Ontario School of Medicine. She also holds a Bachelor’s Degree in Human Nutritional Sciences and a Bachelor of Science in Biology from the University of Manitoba. With over six years of experience as a Clinical Dietitian at the Winnipeg Regional Health Authority, Michelle has extensive knowledge in nutrition education and food services. She has also served as the Director of the Food and Nutrition Services Department, where she led numerous initiatives to improve patient care through targeted nutrition strategies. She is the founder of two elderly nutrition-focused health blogs, The Dietitian Prescription and The Long Term Care RD. Through these platforms, she creates engaging and informative content that bridges the gap between scientific research and practical dietary choices. She is passionate about promoting health through evidence-based nutrition advice, specializing in high protein, high fiber, and low Glycemic Index cooking. Her expertise has been recognized by prominent media outlets, including Forbes, Fox News, Men’s Health, Yahoo, MSN, She Finds, Eat This Not That!, U.S. News and World Report, and AskMen.com. She has also been a featured guest speaker at esteemed events such as the North West Renal Dietitian's Annual Conference and the Dietitians of Canada Annual Conference, where she presented her thesis research.


Unlock expert insights and tips with our exclusive ebook. Enter your email to get your free copy.
Please check your email for a welcome message from Modern60. If it's not in your inbox, kindly check your spam or junk folder
There are no comments yet